Attachment is the two-way bond that develops between you and your baby as you communicate with each other by touch as well as talking. Strong attachment helps your baby's brain to grow, particularly the part of the brain that is important for communicating and forming relationships with others. Your baby feels safe, secure and loved and so learns to love others.
Feeding is a really important time for developing this bond whether you choose to breast or bottle feed. It isn't just about giving your baby energy to grow into a healthy child and adult. Responsive feeding describes how you recognise and respond to your baby's hunger signals or 'cues'. Hold your baby close to you, make eye contact and talk in a loving way. Learn to understand when your baby is no longer hungry and trust your baby's feeling of fullness. Sometimes your baby will only want to feed for a few minutes, sometimes for much longer, in the same way we sometimes just want a drink and a quick snack and at other times a three course dinner!
There are a few differences between responsive breast and bottle feeding:
Responsive breastfeeding
- a baby will not breastfeed if they do not want to, so it is fine to offer the breast whenever you or your baby wish, including when your baby seems distressed. Breastfed babies are in control of their feeding and cannot be overfed or 'spoiled' by frequent feeding. A sit down and a cuddle, even if they do not take much milk, will help your baby develop trust and security.
- On the other hand parents often worry that they do not know how much milk a breastfed baby is taking. Part of this is learning to trust your body and to trust your baby to know what they need. You should expect support from your midwife and health visitor to learn how to know your baby is feeding well by knowing, for example, how many wet & dirty nappies to expect.
Responsive bottle feeding
- When a bottle is put into your baby's mouth, milk comes out of the teat with little or no effort from the baby. As the milk touches the back of the tongue, it triggers the swallow reflex and your baby has to swallow the milk to avoid choking. It is easy to interpret this as a signal that your baby is definitely hungry. For this reason it is very easy to over-feed a baby from a bottle whether it contains formula or expressed breastmilk. this puts your baby at risk of gaining too much weight.
- So it is important to recognise when your baby is getting full. This is easier to do by "pacing". This means letting your baby pause every few sucks to see if they want to stop feeding, taking the bottle out of your baby's mouth and then only starting again if they draw the teat into their mouth themselves. Never force the teat into your baby's mouth or keep trying to feed if your baby turns their head away or pushes the teat out with their tongue. If the bottle is still half full so be it.
- To help attachment keep the number of people who feed your baby to a minimum - ideally just you and your partner or one other close family member.
Responsive feeding of expressed and formula milk:
- Hold your baby close to you, look into their eyes to help them feel safe and loved.
- Hold your baby fairly upright, with their head supported in a comfortable, neutral position.
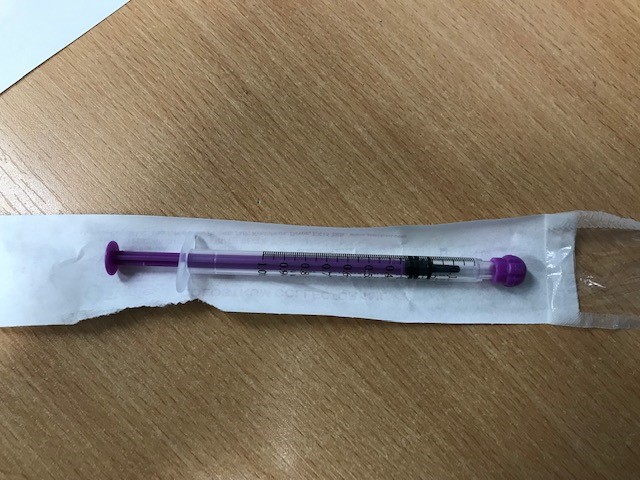
- Rub the teat gently against your baby's lips to encourage them to open their mouth wide and draw the teat into their mouth. Do not force the teat into your baby's mouth.
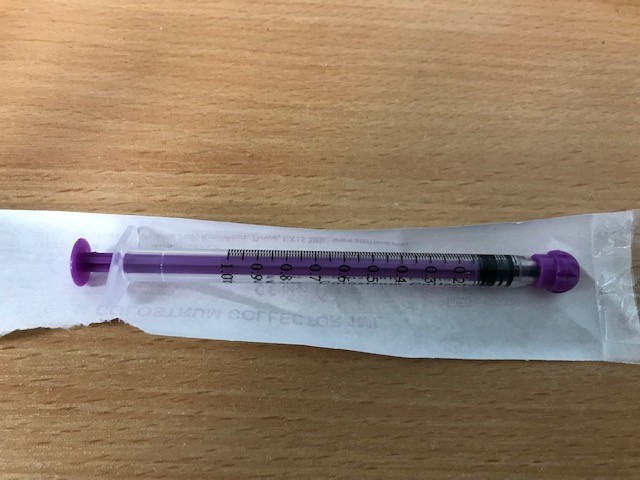
- Hold the bottle level, in line with the ground (horizontal), and then tilt the bottle upwards enough to ensure your baby is taking in milk and not air through the teat.
- Babies feed in bursts of sucking, swallowing and short rests. As your baby is in a fairly upright position, when they pause for a rest the milk will stop flowing allowing them to decide when they are ready to start sucking again.
- During the feed you will see bubbles in the bottle. If you can't see any bubbles, break the suction between your baby's tongue and the teat by moving the teat slightly to the side of their mouth. You should then see bubbles rushing back up into the remaining milk.
- Interrupting the feed from time to time gives your baby a chance to register how full they are and allows them to control what they want. It also gives them the chance to bring up any wind.
- Try to keep the number of people who feed your baby to as few as possible. If another close family member gives an occasional feed, make sure they use the same technique as you so that your baby does not feel frightened or confused.
- Your baby should always be held and never left unattended while feeding from a bottle.
- Do not try to make your baby finish the bottle if it is clear they have had enough.
- Do not use a fast flow teat as babies can find it difficult to control their breathing if they are forced to swallow large volumes of milk quickly.
TOP TIP when bottle feeding:
Hold your baby in an upright position and keep the bottle more horizontal rather than facing downwards. Stop the feed regularly to give your baby a rest.