Childhood Vaccinations - Essential information
Pregnancy
Whooping cough (pertussis) rates have risen sharply in recent years and babies who are too young to start their vaccinations are at greatest risk.
Young babies with whooping cough are often very unwell and most will be admitted to hospital because of their illness. When whooping cough is particularly severe, they can die.
Pregnant women can help protect their babies by getting vaccinated – ideally from 16 weeks up to 32 weeks pregnant. If for any reason you miss having the vaccine, you can still have it up until you go into labour.
Vaccines during pregnancy
The NHS offers pregnant women vaccinations that help protect them and their babies during and after pregnancy. Vaccines help the bodies natural defence system (the immune system) to develop protective antibodies. Antibodies fight disease and produce longer term protection against a particular disease. So, if someone is vaccinated against a particular disease and they come into contact with it at a later date, their immune system will respond to that infection more quickly. Antibodies developed while pregnant pass onto the unborn baby and help to protect them in their first few months of life. Vaccination can help prevent disease or make the illness less serious.
 NHS Website - Whooping Cough Vaccination in Pregnancy
NHS Website - Whooping Cough Vaccination in Pregnancy
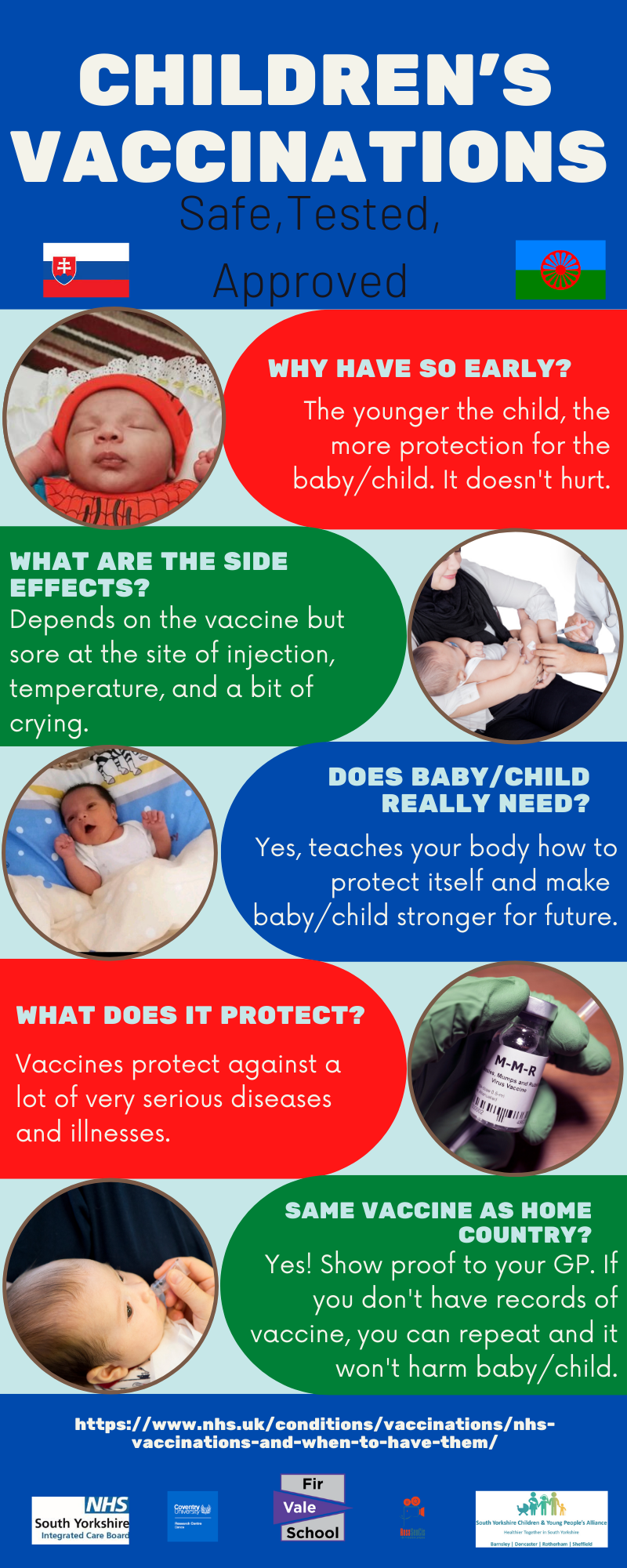
Childhood Vaccinations
We know your child’s health is your top priority and so protecting them from serious disease is incredibly important. That is why the NHS offer a free childhood vaccine programme, protecting your child from certain illnesses.
A vaccine is a type of medicine that trains the body’s immune system so that it can fight a disease it has not come into contact with before. Vaccines are designed to prevent disease, rather than treat a disease once you have caught it.
Because vaccines have been used so successfully in England, they prevent more than 5,000 deaths and more than 100,000 hospital admissions each year.
Infections like measles and whooping cough can have a huge impact on your child’s life. They can miss out on school due to time spent unwell, be hospitalised, and even experience life-long complications, disability and in some cases tragically can cause death.
All childhood vaccinations offered by the NHS have been used in millions of children and have an excellent safety record. All health authorities worldwide agree that immunisation is the safest way to protect our children’s health. If you do have any questions, do not hesitate to speak to your GP or health visitor – they will be happy to address any concerns and guide you through your vaccination schedule.
Information source: UK Health Security Agency (UKHSA) Childhood immunisations campaign 2024
Content reviewed by: NHS England (NHSE) Screening and Immunisation Team
The current routine childhood immunisation schedule
Flu and Covid-19 Vaccines
Flu can be very unpleasant for children and can sometimes cause serious problems, such as pneumonia. Children can catch and spread flu easily. Vaccination also helps protect others who are higher risk of getting seriously ill from flu, such as babies and older people by reducing the spread of it.
The children’s flu vaccine is offered on the NHS every year in autumn or early winter. It is recommended for:
- Children aged 2 or 3 years
- School-aged children (Reception to Year 11)
- Children aged 6-month up to 18 years with certain long-term health conditions
If your child is 2 or 3 as of 31st August, they will get the flu vaccine at their GP surgery. Your local GP surgery should invite you, or you can contact them to book an appointment.
The flu vaccine is offered to all school-aged children from Reception to Year 11 via the school immunisation team, this includes children not educated in a school setting. The school immunisation team will work with the school to send you an invite for your child's vaccine, usually in the autumn term. If your child does not get their vaccine at school or if they learn at home, a community clinic should offer them a flu vaccine. If your child has turned 4 years old but was 3 years old on 31st August but have not started school yet, they can get the flu vaccine from their GP surgery. If they were 4 years old on 31st August the school immunisation team will arrange vaccination, even if they have not started school yet.
Children with certain long-term health conditions that put them at higher risk from flu can get a flu vaccine from their school immunisation team (if they're in Reception to Year 11) or GP surgery.
Information source: UK Health Security Agency (UKHSA) Childhood immunisations campaign 2024
Content reviewed by: NHS England (NHSE) Screening and Immunisation Team
MMRV Vaccine
Measles is highly infectious and spreads easily (when an infected person breathes, coughs or sneezes) among those who are unvaccinated. Measles can be a very unpleasant illness. In some children it can be serious and lead to hospitalisation – and in rare cases tragically can cause death. People in certain risk groups including babies and young children, pregnant women, and people with weakened immunity, are at increased risk of complications from measles.
Symptoms include a runny nose, cough, high fever, sore red watery eyes and a blotchy red-brown rash.
These infections spread very easily between people and can lead to serious problems including menningitis, inflammation of the brain (encephalitis), pneumonia, and hearing loss.
The number pf doses children are given depends on when they were born. Some older children will have already had 1 or 2 doses of the MMR vaccine which also protects against Measles, Mumps, Rubella but not chickenpox. MMRV vaccine at the right time (2 doses at 1 year old and 18 months old for anyone born aftrer January 202) is the best way to protect your child and help prevent it spreading, especially to those most vulnerable. Two doses of the MMRV vaccine give you excellent lifelong protection. - see https://.www.nhs.uk/vaccinations/mmrv-vaccine/
Some years ago, there were stories suggesting a link between the MMRV vaccine and autism. All medical authorities agree that no such link exists.
HPV Vaccine
HPV vaccine overview
Girls and boys aged 12 to 13 years (born after 1 September 2006) are offered the human papillomavirus (HPV) vaccine as part of the NHS vaccination programme.
The HPV vaccine helps protect against cancers caused by HPV, including:
- cervical cancer
- some mouth and throat (head and neck) cancers
- some cancers of the anal and genital areas
It also helps protect against genital warts.
In England, girls and boys aged 12 to 13 years are routinely offered the 1st HPV vaccination when they're in school Year 8. The 2nd dose is offered 6 to 24 months after the 1st dose.
It's important to have both doses of the vaccine to be properly protected.
If you’re eligible and miss the HPV vaccine offered in Year 8 at school, it’s available for free on the NHS up until your 25th birthday for:
- girls born after 1 September 1991
- boys born after 1 September 2006
What is HPV?
HPV is the name given to a very common group of viruses.
There are many types of HPV, some of which are called "high risk" because they're linked to the development of cancers, such as cervical cancer, anal cancer, genital cancers, and cancers of the head and neck.
Other types can cause conditions like warts or verrucas.
High risk types of HPV can be found in more than 99% of cervical cancers.
There is also a significant association between HPV and some of the anal and genital cancers, and cancers of the head and neck.
HPV infections do not usually cause any symptoms, and most people will not know they're infected.
Vaccinations for at-risk babies and children
There are some vaccines which are available on the NHS to those who need extra protection.
|
At-risk group |
Vaccines |
|
Babies born to mothers who have hepatitis B |
Hepatitis B vaccine at birth, 4 weeks (then doses contained within routine childhood programme) and 12 months |
|
Infants born in areas of the country where there are high numbers of TB cases (if unsure speak to your midwife) |
BCG tuberculosis (TB) vaccine at or by 28 days |
|
Infants whose parents or grandparents were born in a country with many cases of TB |
BCG tuberculosis (TB) vaccine at around 4 weeks |
|
Children 6 months to 17 years old with long-term health conditions |
Children's flu vaccine every year |
How to book your child’s Vaccination appointment
All the childhood vaccinations are free. You will be contacted by your GP surgery and/or the local Child Health Information Service when your child is due a routine immunisation – this could be by letter, phone, text or email. If your child has missed any vaccinations, then it is best to speak to your GP surgery. While it is best for your children to have their vaccinations as per the NHS vaccination schedule, it is never too late to check if they can still have them.
Your local school aged immunisation service may also offer community clinics and/or home visits:
Barnsley School Aged Immunisation Service
Doncaster School Aged Immunisation Service
FAQs
Is it safe to have several vaccinations in one go?
Yes. From birth, babies’ immune systems protect them from the germs that surround them. Without this protection, babies would not be able to cope with the tens of thousands of bacteria and viruses that cover their skin, nose, throat and intestines. This protection carries on throughout life.
Studies have shown that it is safe to have several vaccinations at the same time and your baby will be protected as soon as possible from some very serious infections.
My child is unwell – can they still go for their vaccination?
If your child has a minor illness without a fever, such as a cold, they should have their vaccinations as normal.
If your child is ill with a fever, put off the vaccination until the child has recovered (your practice nurse or GP or Health Visitor will be able to advise). This is to avoid the fever being associated with the vaccine, or the vaccine increasing the fever your child already has.
Why does my child need multiple doses of some vaccines?
Most vaccinations have to be given more than once to ensure your child’s immunity is as high as possible. For example, 3 doses of DTaP/IPV/Hib/HepB vaccine are needed to provide protection in babies.
How do we know that vaccines are safe?
Before a vaccine is allowed to be used, its safety and effectiveness have to be thoroughly tested. After they have been licensed, the safety of vaccines continues to be monitored. All routine vaccines in the NHS programme have been used in millions of children worldwide and have an excellent safety record.
All health authorities worldwide agree that vaccination is the safest way to protect our children’s health
Will there be any side effects from the vaccines?
Any side effects that occur are usually mild and short lived. Your child may get a little redness, swelling or tenderness where the injection was given that will disappear on its own. Fever can be expected after any vaccination.
Advice for parents on what to expect after vaccination.
Fever is more common after the first two doses of the Meningococcal B (Men B) vaccination, which are given at 8 weeks and 16 weeks old. There is specific advice for parents on how to prevent and treat fever after MenB vaccine at 8 and 16 weeks here: MenB vaccine and paracetamol
I’m worried that my child may have allergies. Can they be vaccinated?
Very rarely, children can have an allergic reaction soon after vaccination. This reaction may be a rash or itching affecting part or all the body. You should report this to the doctor or nurse giving the vaccine who will advise you on how to treat this. It does not mean that your child should stop having all vaccinations. Any reaction will be discussed and assessed before giving any future vaccines.
Anaphylactic reaction
Even more rarely, children can have a severe reaction, within a few minutes of the vaccination, which causes breathing difficulties and can cause the child to collapse. This is called an anaphylactic reaction. A recent study has shown that there is only 1 anaphylactic reaction in about a million vaccinations.
An anaphylactic reaction is a severe and immediate allergic reaction that needs urgent medical attention. The people who give vaccination are trained to deal with anaphylactic reactions and most children recover completely with treatment.
What if my child has an underlying health condition?
There are very few reasons why babies and children cannot be immunised. Vaccines should not be given to babies or children who have had a confirmed anaphylactic reaction to either a previous dose of the vaccine, or to any contents of that vaccine. The Nurse or Doctor doing the vaccination will have all this information available to them.
Immunosuppressed children
In general, children who are ‘immunosuppressed’ should not receive certain live vaccines.
Children who are immunosuppressed include those whose immune system does not work properly because they are undergoing treatment for a serious condition such as a transplant or cancer, or who have any condition which affects the immune system, such as severe primary immunodeficiency. Primary immunodeficiencies are very rare diseases that mean you are more likely to catch infections. They are usually caused by a faulty gene and are diagnosed soon after birth
If this applies to your child, you must tell your doctor, practice nurse or health visitor before the vaccination. These children can be best protected by ensuring those around them, for example their siblings, are fully vaccinated.
They will need to get specialist advice on using live vaccines such as MMR, rotavirus vaccine and Bacillus Calmette-Guérin vaccine (BCG).
There are no other reasons why vaccines should definitely not be given.
Some individuals who have compromised/impaired immune systems may not make a full response to the vaccine, and additional doses may be required. Your Doctor or Nurse will be able to advise.
What about the MMR and nasal spray fu vaccine? Are there any other reasons why my child should not receive these?
The MMR and nasal flu vaccines are live attenuated vaccines (that is, they contain viruses that have been weakened). Children who are ‘immunosuppressed’ may not be able to receive one or both of these live vaccines. Children who are immunosuppressed include those:
- whose immune system is suppressed because they are undergoing treatment for a serious condition such as a transplant or cancer, or
- who have any condition which affects the immune system, such as severe primary immunodeficiency. If this applies to your child, you must tell your doctor, practice nurse, school nursing team or health visitor before the vaccination. They will get specialist advice.
Can I check my child is up to date with their vaccinations?
If you are not sure if your child has had all their routine vaccinations, check their personal health record (Red Book) or contact the GP surgery.
If your child is going abroad, make sure their routine vaccinations are up to date. Your child may also need extra vaccinations e.g if any have to be given early, they may need repeating when you return, and you may also need to take other precautions.
How will I know when my baby’s vaccinations are due?
Your doctor’s surgery or clinic or child health information service will send you a letter and/or an appointment for you to bring your baby for their vaccinations. Most surgeries and health centres run special vaccination or baby clinics. If you can’t get to the clinic, contact the surgery to make another appointment. All childhood vaccinations are free. You can also find details in your child’s Red Book.
How can I catch up if my child has missed any vaccinations?
If you miss the appointment or need to delay the vaccination, make a new appointment. You can pick up the immunisation schedule where it stopped without having to start again, although your child may no longer be eligible for some vaccines
Do any routine childhood vaccines contain pork?
Gelatine is a substance derived from the collagen of animals such as chickens, cattle, pigs and fish. Porcine gelatine is used in some vaccines as a stabiliser. This is to ensure that the vaccine remains safe and effective during storage. Porcine gelatine is found in two of the vaccines routinely given to children: one of the MMR vaccines and the nasal influenza vaccine.
In the UK we have two MMR vaccines, both of which work equally well, one contains porcine gelatine and the other doesn’t. If you want your child to have the porcine gelatine free vaccine discuss it with your practice nurse or GP or school immunisation team.
What is the whooping cough vaccine?
Please click here for a fact sheet on whooping cough and the whooping cough vaccine
Protecting Our Future: Fir Vale Students Speak Out on HPV Vaccination